The commonwealth Fund report 2024
The report reveals the well known and painful truth again for the most powerful and wealthy country in the world…
Mirror, Mirror 2024: An International Comparison of Health Systems | Commonwealth Fund
Coronary sinus reducer for the treatment of refractory angina (ORBITA-COSMIC)
Atrial flutter with 1:1 AV conduction, a case series
Cardiology Journal Watch 9th Feb 2024
Cardiology Journal watch 9th Feb 2024
Debjit Chatterjee
ORBITA2
Dec 2023 NEJM
Among patients with stable angina who were receiving little or no antianginal medication and had objective evidence of ischemia, PCI resulted in a lower angina symptom score ( improvement in angina) than a placebo procedure
– double-blind, randomized, placebo-controlled trial
-300 patients randomised to either PCI or placebo procedure in 1: 1 ratio
– All patients had non-invasive evidence of ischaemia before coronary angiogram
-Follow up for 12 weeks (1)
In an editorial regarding the above study in NELM, the comments are (2)
The ORBITA-2 trial will influence patient care, guidelines, and the design of new trials. one can think now of two evidence-based pathways for the management of stable angina:
-initial medical therapy, and then PCI if the medical therapy fails to relieve symptoms or if the patient develops unacceptable side effects from antianginal medication,
-or PCI without the use of antianginals with the addition of medical therapy if the symptoms continue.
-The pros and cons of both pathways should be discussed with the patient, including the risks of PCI, the chance of stent thrombosis (0.5% per year), and the need for dual antiplatelet therapy with the associated risk of bleeding.
Patients should express a preference, which is important.
Angiographic findings may tilt the decision towards one or other. Implanting a stent in a small branch vessel in a patient who has a high risk of stent thrombosis may be inappropriate
References-
- Rajkumar CA, Foley MJ, Ahmed-Jushuf F et al A Placebo-Controlled Trial of Percutaneous Coronary Intervention for Stable Angina, for the ORBITA-2 Investigators. n engl j med 389;25 nejm.org December 21, 2023
- Changing the Orbit around Percutaneous Coronary Intervention for Stable Angina Harvey D. White, D.Sc. n engl j med 389;25 nejm.org December 21, 2023
ARTESIA
January 11 , 2024 NEJM
Among patients with subclinical atrial fibrillation, apixaban resulted in a lower risk of stroke or systemic embolism than aspirin but a higher risk of major bleeding
Subclinical AF = Any AF detected in Pacemaker or ICD of 6miniutes to 24 hours duration
Total of 4012 patients
Mean CHA2DS2VASc Was 3.9 +_ 1.1
Mean follow up 3.5 +_ 1.8 years
Stroke or systemic embolism occurred in 0.78% per patient year in apixaban group versus 1.24% per patient year P= 0.007
Major bleeding happened in 1.71% per patient year versus 0.94% per patient year in aspirin group P = 0.001. Fatal bleeding occurred in 5 patients in apixaban group versus 8 patients in aspirin group (1)
Compare this results with another similar trial— NOAH-AFNET6 ( published in Sept 2023 in NEJM) in similar group of patients , edoxaban, as compared with placebo, did not provide a benefit with respect to the primary efficacy outcome (Stroke, systemic embolism , cardiovascular death) and was associated with a higher incidence of a composite of death or major bleeding. Analysis of stroke was underpowered because of small number of stroke. (2)
References-
1.Healey JS, Lopes RD, Granger CB et al .Apixaban for Stroke Prevention in Subclinical Atrial Fibrillation. For the ARTESIA Investigators. N Engl J Med 2024; 390:107-117 DOI: 10.1056/NEJMoa2310234
- Kirchhof P, Toennis T, Goette A, et al. Anticoagulation with edoxaban in patients with atrial high-rate episodes. N Engl J Med 2023;389:1167-79.
Interaction of iPhone 12 with cardiac implantable electronic devices: is it of any clinical concern?
Two articles have been published recently as ‘letters to the editor’ in Heart Rhythm online, about the effect of the newly released iPhone 12 on the function of cardiac implantable electronic devices (CIED), if it is held close to a device. In one article, Greenberg et al.¹ first reported inhibition of tachycardia therapy of a Medtronic implantable cardioverter-defibrillator (ICD) when iPhone 12 was kept close to the device. In the second article, Patterson et al.² compared the effect of iPhone 12 and iPhone XS on CIED of different types and models from different manufactures. The authors of these articles have now conclusively documented that the newly released iPhone 12 can interfere with the function of CIED significantly. iPhone 12 temporarily but consistently inhibited detection of tachyarrhythmia, and hence delivery of appropriate therapy in some models of ICD/cardiac resynchronisation therapy defibrillator. In case of pacemakers, one model (Assurity DR, Abbott) went into asynchronous mode when iPhone 12 was held close to the device. This has caused a huge stir among the cardiologists, common people, and patients with CIED. The overwhelming question now is whether this is going to be a significant public health issue
EP Europace, Volume 24, Issue 2, February 2022, Pages 179–180, https://doi.org/10.1093/europace/euab159
A rare coronary angiogram
A 35-year-old woman was admitted with atypical chest pain. Her electrocardiogram was normal. There was no rise in serum troponin level. Echocardiogram showed a structurally normal heart with preserved left ventricular systolic function. Her serum cholesterol was very high (total cholesterol of 7.7 mmol/L with LDL of 5.3 mmol/L) but there was no other conventional risk factor for coronary artery disease. In view of ongoing chest pain and high cholesterol, a coronary angiogram was done to rule out coronary artery disease (Figures 1 and 2; Supplementary material online, Videos S1 and S2). Answer: 3. Anomalous origin of left coronary artery from right sinus of Valsalva with retro-aortic course. Explanation Origin of the left main coronary artery (LMCA) from the right sinus of Valsalva is a rare congenital anomaly with an estimated incidence of 0.04%. It has been associated with sudden cardiac death in young persons. Identification of the course of the LMCA after its origin is important to stratify the risk of sudden death. A computed tomography coronary angiogram (CTCA) will identify the course of the LMCA after its origin but in 1985 Ishikawa et al. 1 described a method to determine the course of the LMCA by conventional invasive Figure 2 Left anterior oblique view. Figure 1 Right anterior oblique view.
European Heart Journal. Acute Cardiovascular Care, Volume 11, Issue 5, May 2022, Pages e2–e3, https://doi.org/10.1093/ehjacc/zuac030
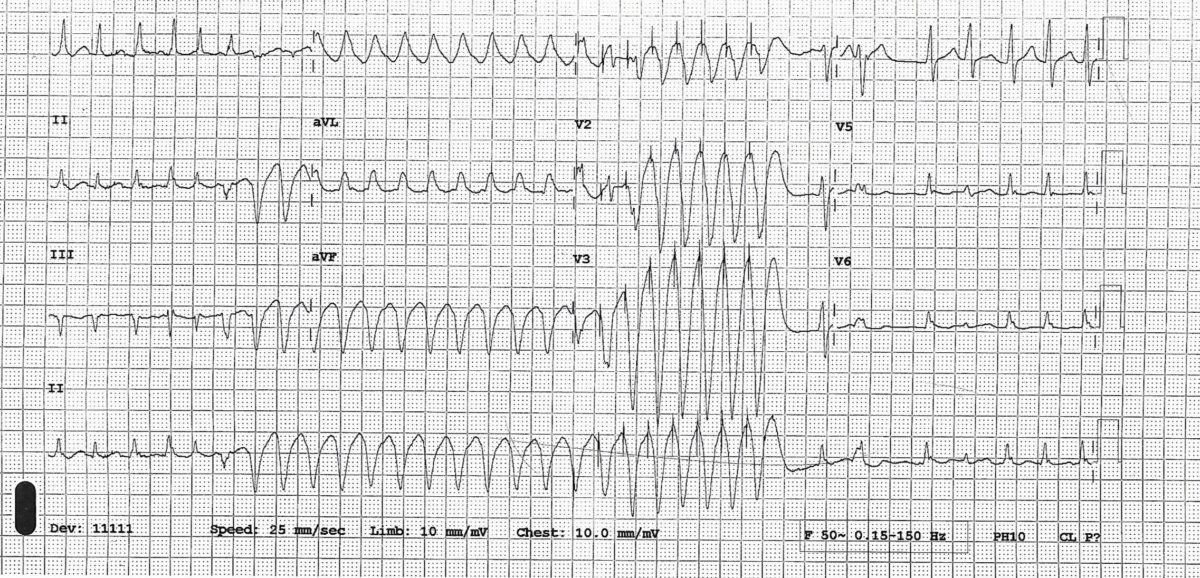
A broad complex tachycardia in a patient on flecainide
This is an interesting case of wide complex tachycardia in a patient on flecainide for paroxysmal atrial fibrillation. Diagnostic possibilities were discussed, actual diagnosis revealed, and explanation provided.
July 2021Br J Cardiol 2021;28:119–20doi:10.5837/bjc.2021.034
Case of the month 2
A 71-year-old woman presented to the emergency department (ED) with weakness, dizziness and some episodes of cardiac sounding chest pain for few days. There was no history of diabetes or hypertension and she was a non-smoker.
She saw a cardiologist for dizziness about a year ago. Her ECG showed frequent ventricular ectopics and echocardiogram showed structurally normal heart with preserved LV function and hence she was reassured cardiac wise at that stage. Her dizziness was subsequently thought to be vertigo.
This time she thought her dizziness to be exacerbation of her usual vertigo but episodes of chest pain made her seek medical advice. She was known to have ulcerative colitis and was on mesalazine. On presentation to ED , her hs troponin was 541 (normal < 14). ECG showed T wave inversion in V1-V4.
ECG-

In view of chest pain, increased troponin and ECG changes she was treated as acute coronary syndrome (NSTEMI) and had a coronary angiogram done which showed normal coronary arteries. An echocardiogram showed dyskinesia of the mid and apical part of the LV ventricle with hypercontractile basal segment.
This echo feature is typical of something called Takotsubo cardiomyopathy (because it resembles an octopus pot) or apical ballooning syndrome. See video and still images
This condition was first described in 1990.This happens predominantly in post-menopausal women after severe mental or physical stress and hence is also called broken heart syndrome. There was no obvious trigger in our case. In an international registry of Takotsubo cardiomyopathy patients of 1758 patients 28.5% had no preceding trigger. (1)
- Modified Mayo clinic diagnostic criteria for Takotsubo cardiomyopathy. Patients are assigned this diagnosis when they satisfy all criteria
(1) Transient hypokinesis, akinesis, or dyskinesis in the left ventricular mid segments with or without apical involvement; regional wall motion abnormalities that extend beyond a single epicardial vascular
distribution; and frequently, but not always, a stressful trigger
(2) Absence of obstructive coronary disease or angiographic evidence of acute plaque rupture
(3) New ECG abnormalities (ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin
(4) Absence of pheochromocytoma and myocarditis. - The prognosis is usually favourable and the LV function improves in 4-8 weeks’ time. Complications can happen in up to 20% patients and can include shock, thrombus formation, heart failure, cerebrovascular
accident, ventricular tachycardia, left ventricular rupture and/or ventricular septal rupture. In our patient an echocardiogram done after 3 weeks showed LV function had almost returned to normal
(see video below) - Treatment is usually supportive (treatment of heart failure and arrhythmia and anticoagulation if LV thrombus develops)
- There is a small chance of recurrence
The first video shows echocardiogram on this presentation
The second video is echo after 3 weeks
Compare the contraction of mid and apical part of LV in 2 videos
Echo after 3 weeks
Reference:
1. Templin C, Ghadri JR, Dikeman J et al. Clinical features and outcomes of Takotsubo (stress) cardiomyopathy. NEJM 2015;373(10):929-38.
2. Yoshihiro J. Akashi, David S. Goldstein, Giuseppe Barbaro and Takashi Ueyama Takotsubo Cardiomyopathy : A New Form of Acute, Reversible Heart Failure. Circulation. December 16/23, 2008,Volume 118, Issue 25
Case of the month 1
A 49-yr-old woman presented to her general practitioner (GP) with shortness of breath on exertion and mild ankle swelling for few weeks. She was a smoker and initial impression was that she probably suffered from smoking induced chronic obstructive pulmonary disease. Her BNP was slightly raised at 156 pg/ml and hence her GP requested for an open access echocardiogram (TTE) which showed a mass in left atrium. A transoesophageal echocardiogram (TOE) was arranged for further evaluation and it showed the following-
As you can see in transoesophageal echocardiogram, there was a mass in left atrium attached to interatrial septum with a stalk and projecting into the left ventricle through the mitral valve causing obstruction in mitral inflow in diastole. This echo appearance is typical of left atrial myxoma.
- Myxoma is the most common primary cardiac tumour and accounts for 30-50% of all primary tumours pf the heart. Myxomas are usually single and occur in the left atrium in 75% cases where they most commonly arise from the area of fossa ovalis. Rarely myxoma can be a part of Carney Syndrome (Autosomal dominant, multiple myxoma formation in cardiac and exrtracardiac tissue, spotty skin pigmentation, endocrine hyperactivity, other tumours like testicular tumour and pituitary adenoma). On echocardiogram myxomas can appear smooth surfaced but is more commonly irregular. They are typically nonhomogeneous in texture with lucent centres or areas of calcification.
- Annual incidence is around 0.5 per million population (1)
- Majority of the patients present with one or more of the classic triad of obstructive, embolic or constitutional features
Obstructive symptoms and signs–dizziness, sob, cough, pulmonary oedema and heart failure due to obstruction to mitral inflow by the tumour
Embolic manifestations — due to tumour embolism to systemic or pulmonary circulation depending on the location of the tumour
Constitutional features– fever, weight loss, fatigue, myalgia, arthralgia, muscle weakness, Raynaud’s syndrome. They are believed to be due to IL-6 released by myxoma tumour cells (2).
- Transthoracic /trans-oesophageal echo is diagnostic in typical cases. TOE is more sensitive and specific compared to TTE. CT and Cardiac MR are helpful in case of small tumours and in cases with atypical appearances
- Treatment is surgical removal as early as possible. There is about 3% chance of recurrence in sporadic cases though a more recent report found no recurrence after a mean follow up 72 months after surgical excision in 82 cases of LA myxoma (3). Chance of recurrence is higher in familial cases (20%)
References–
- MacGowan SW, Sidhu P, Aherne T, Luke D, Wood AE, Neligan MC, McGovern E. Atrial myxoma : national incidence, diagnosis and surgical management. Ir J Med Sci. 1993 Jun;162(6):223-6.doi: 10.1007/BF02945200
- Mendoza CE, Rosado MF, Bernal L. The role of interleukin-6 in cases of cardiac myxoma. Clinical features, immunologic abnormalities, and a possible role in recurrence. Tex Heart Inst J. 2001. 28(1):3-7.
- Vroomen M, Houthuizen P, Khamooshian A, Soliman Hamad MA, van Straten AH. Long-term follow-up of 82 patients after surgical excision of atrial myxomas. Interact Cardiovasc Thorac Surg. 2015 Aug. 21 (2):183-8.

 in diastole
in diastole in systole
in systole