Category: ECG teaching
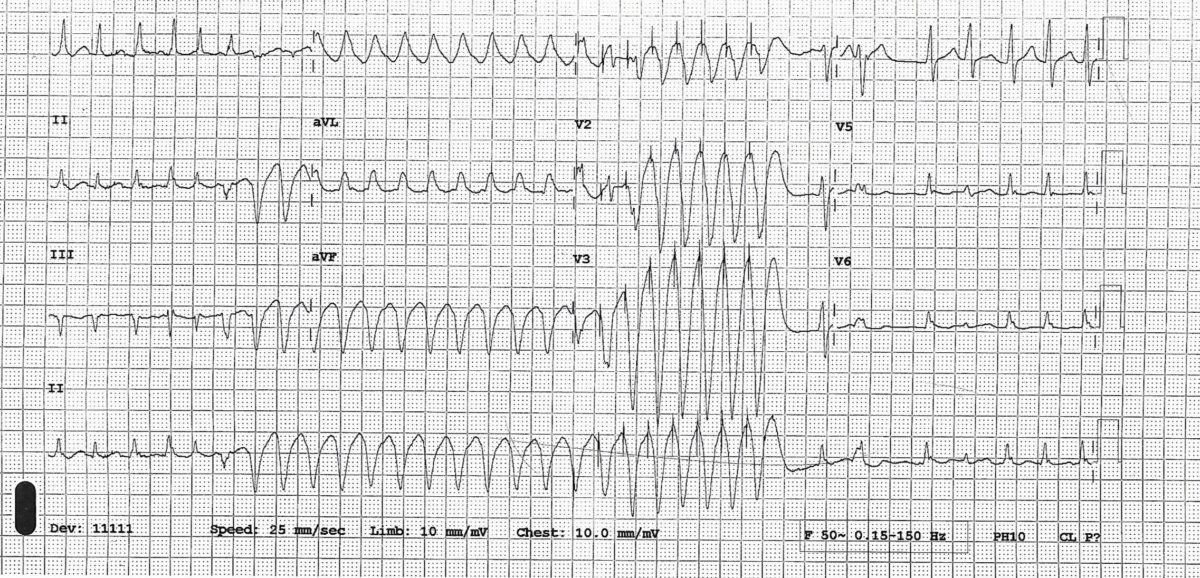
A broad complex tachycardia in a patient on flecainide
This is an interesting case of wide complex tachycardia in a patient on flecainide for paroxysmal atrial fibrillation. Diagnostic possibilities were discussed, actual diagnosis revealed, and explanation provided.
July 2021Br J Cardiol 2021;28:119–20doi:10.5837/bjc.2021.034
ECG of the week 3
A 22-yr-old man presented to emergency department with acute onset sharp pain across his chest with some radiation to neck. Intensity of the pain did not change with respiration though there was some relief on bending forward. On direct questioning he admitted having sore throat for last 2 days. There were no conventional risk factors for coronary artery disease. On examination there was no murmur or rub.
ECG on the day of admission (ECG 1)
Troponin went from 772 to 1955 (normal up to 13.9), WBC 10.2 ( Normal 4- 10) Neutrophil 7.5 ( Normal 2- 7) CRP not requested
Echo on admission showed bright pericardium with some hypokinesia of LV apical segment. Overall LV function was mildly impaired
ECG after 48 hours (ECG 2)
ECG 1

ECG 2

A diagnosis of myopericarditis was made. Chest pain and ECG changes were suggestive of pericarditis and high troponin and echo findings were evidence of myocardial involvement.
He was treated with ibuprofen and colchicine and was discharged with plan for outpatient cardiac MRI and review in clinic. He was asymptomatic at discharge.
Learning points
1. What did ECGs show? (see the ECG explained below)
ECG 1 showed global concave up ST elevation with reciprocal depression in lead aVR and V1, depressed PR segment (measured from baseline TP segment)
Changes evolved into ECG 2 which showed T wave inversion. Inverted T waves could be evolving changes of pericarditis but sometimes they may be manifestations of myocardial involvement.
Though ECG changes of pericarditis are classically described in 4 stages, not every patient goes through all stages and the duration of each stage varies between patients.

2. What are the differential diagnosis of this ECG?
STEMI
• Will normally show convex upwards ST elevation though can be concave up
• ST elevation will conform to some arterial territory (anterior, inferior etc.) rather than global though on the other hand ECG changes in the pericarditis can sometimes be localised
• Reciprocal ST depression in leads other than aVR and V1
Early repolarisation
• ST elevation not global (usually inferolateral)
• No PR depression
•No evolution in ST changes over time
ESC guidelines 2015–

ECG of the week 2
This is a straightforward but exceedingly rare ECG.
A 70-yr-old man presented with an episode of collapse. He was known to have severe LV systolic dysfunction and atrial fibrillation for a while. His coronaries were unobstructed, and his ECG showed-

As you can see ECG shows LBBB with right axis and atrial fibrillation. LBBB and right axis is a rare combination. LBBB is usually associated with normal or left axis. LBBB with right axis usually indicates biventricular enlargement and diffuse conduction system disease.
From a database of 636,000 electrocardiograms a series of only 36 patients with this combination was described. Most subjects had dilated cardiomyopathy with biventricular enlargement. (1)
References
1. Childers R1, Lupovich S, Sochanski M, Konarzewska H. Left bundle branch block and right axis deviation: a report of 36 cases. J Electrocardiol. 2000;33 Suppl:93-102.
ECG of the week 1
A 71-yr-old man was admitted with increased shortness of breath and pedal swelling for few days. He was known to suffer from COPD and this admission was thought to be due to acute infective exacerbation. There was no cardiac history. On admission there was significant tachycardia and ECG (ECG 1 and 2) was done. The rhythm was mentioned as atrial fibrillation in his notes. Echocardiogram showed preserved LV systolic function, dilated right ventricle with moderate tricuspid regurgitation, pulmonary artery pressure could not be measured because of poor echo window and TR could only be visualised in subcostal view.
What is the true rhythm in ECG?
ECG 1

ECG 2

The rhythm is multifocal atrial tachycardia (also called chaotic atrial tachycardia) and not AF.
● There are multiple morphologies of P wave (classically described as at least 3 morphologies). PP intervals are irregular; most P waves are conducted to the ventricles though with varying PR intervals leading to irregular RR intervals creating a general impression of AF
● This rhythm usually occurs in older patients with COPD or congestive heart failure and may eventually develop into atrial fibrillation
● Digoxin and theophylline administration can be causally related
● Management is primarily that of underlying disease. Beta blocker is helpful if tolerated but is usually avoided because of associated obstructive airway disease. Non-dihydropyridine calcium channel blockers (diltiazem, verapamil) and amiodarone may be helpful. There is some evidence that IV magnesium may control the rate or even revert it to sinus rhythm.