A 71-year-old woman presented to the emergency department (ED) with weakness, dizziness and some episodes of cardiac sounding chest pain for few days. There was no history of diabetes or hypertension and she was a non-smoker.
She saw a cardiologist for dizziness about a year ago. Her ECG showed frequent ventricular ectopics and echocardiogram showed structurally normal heart with preserved LV function and hence she was reassured cardiac wise at that stage. Her dizziness was subsequently thought to be vertigo.
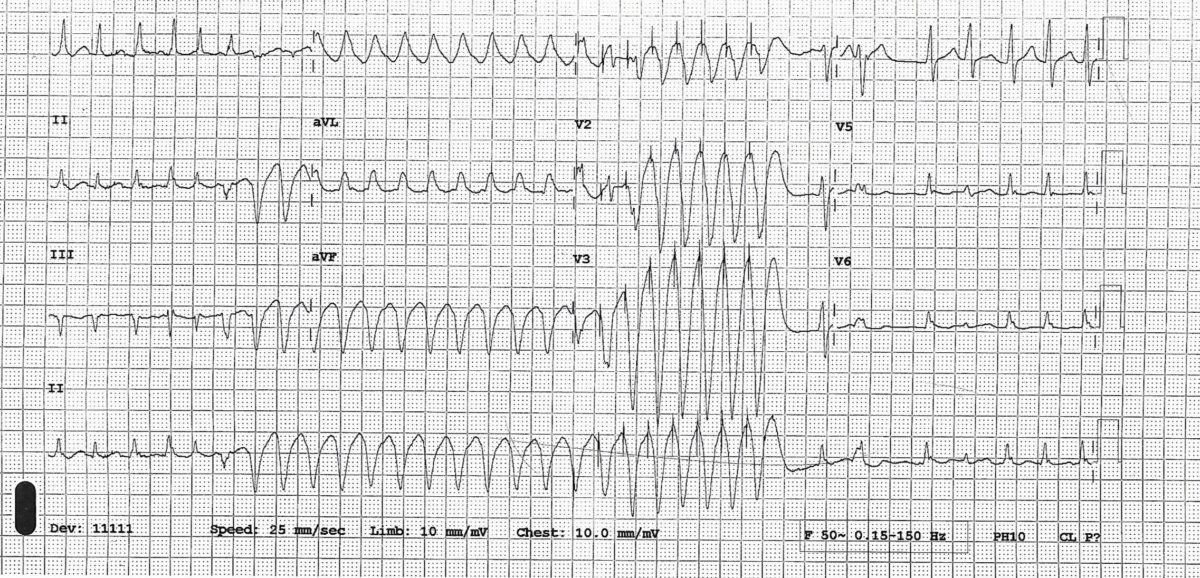
This time she thought her dizziness to be exacerbation of her usual vertigo but episodes of chest pain made her seek medical advice. She was known to have ulcerative colitis and was on mesalazine. On presentation to ED , her hs troponin was 541 (normal < 14). ECG showed T wave inversion in V1-V4.
ECG-

In view of chest pain, increased troponin and ECG changes she was treated as acute coronary syndrome (NSTEMI) and had a coronary angiogram done which showed normal coronary arteries. An echocardiogram showed dyskinesia of the mid and apical part of the LV ventricle with hypercontractile basal segment.
This echo feature is typical of something called Takotsubo cardiomyopathy (because it resembles an octopus pot) or apical ballooning syndrome. See video and still images
This condition was first described in 1990.This happens predominantly in post-menopausal women after severe mental or physical stress and hence is also called broken heart syndrome. There was no obvious trigger in our case. In an international registry of Takotsubo cardiomyopathy patients of 1758 patients 28.5% had no preceding trigger. (1)
- Modified Mayo clinic diagnostic criteria for Takotsubo cardiomyopathy. Patients are assigned this diagnosis when they satisfy all criteria
(1) Transient hypokinesis, akinesis, or dyskinesis in the left ventricular mid segments with or without apical involvement; regional wall motion abnormalities that extend beyond a single epicardial vascular
distribution; and frequently, but not always, a stressful trigger
(2) Absence of obstructive coronary disease or angiographic evidence of acute plaque rupture
(3) New ECG abnormalities (ST-segment elevation and/or T-wave inversion) or modest elevation in cardiac troponin
(4) Absence of pheochromocytoma and myocarditis.
- The prognosis is usually favourable and the LV function improves in 4-8 weeks’ time. Complications can happen in up to 20% patients and can include shock, thrombus formation, heart failure, cerebrovascular
accident, ventricular tachycardia, left ventricular rupture and/or ventricular septal rupture. In our patient an echocardiogram done after 3 weeks showed LV function had almost returned to normal
(see video below)
- Treatment is usually supportive (treatment of heart failure and arrhythmia and anticoagulation if LV thrombus develops)
- There is a small chance of recurrence
The first video shows echocardiogram on this presentation
The second video is echo after 3 weeks
Compare the contraction of mid and apical part of LV in 2 videos
 in diastole
in diastole
 in systole
in systole
Echo after 3 weeks
Reference:
1. Templin C, Ghadri JR, Dikeman J et al. Clinical features and outcomes of Takotsubo (stress) cardiomyopathy. NEJM 2015;373(10):929-38.
2. Yoshihiro J. Akashi, David S. Goldstein, Giuseppe Barbaro and Takashi Ueyama Takotsubo Cardiomyopathy : A New Form of Acute, Reversible Heart Failure. Circulation. December 16/23, 2008,Volume 118, Issue 25


 in diastole
in diastole in systole
in systole