A 71-yr-old man was admitted with increased shortness of breath and pedal swelling for few days. He was known to suffer from COPD and this admission was thought to be due to acute infective exacerbation. There was no cardiac history. On admission there was significant tachycardia and ECG (ECG 1 and 2) was done. The rhythm was mentioned as atrial fibrillation in his notes. Echocardiogram showed preserved LV systolic function, dilated right ventricle with moderate tricuspid regurgitation, pulmonary artery pressure could not be measured because of poor echo window and TR could only be visualised in subcostal view.
What is the true rhythm in ECG?
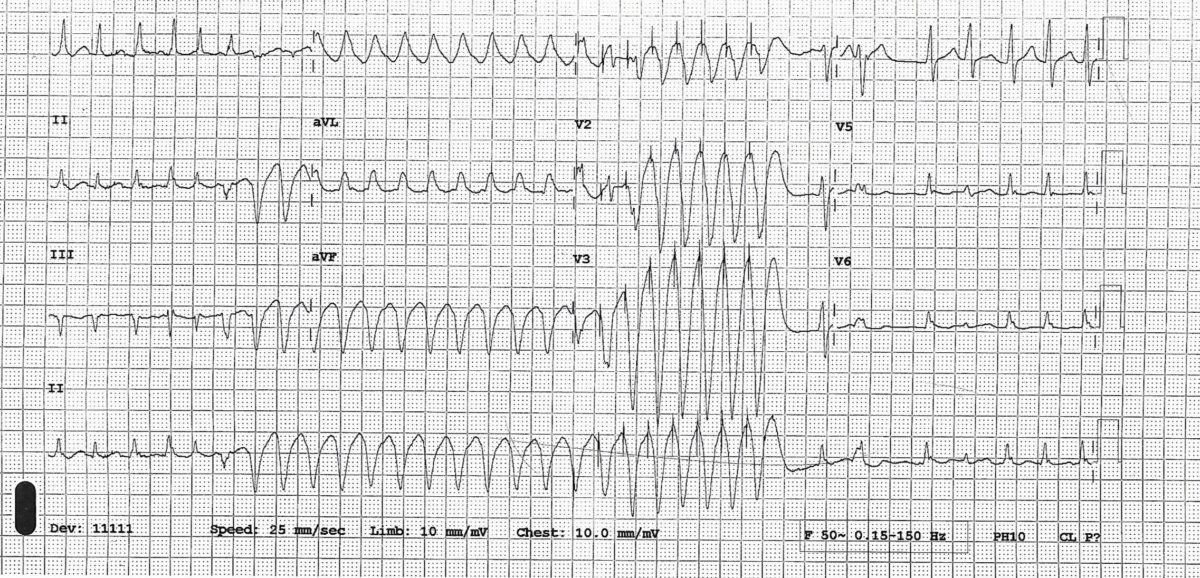
ECG 1

ECG 2

The rhythm is multifocal atrial tachycardia (also called chaotic atrial tachycardia) and not AF.
● There are multiple morphologies of P wave (classically described as at least 3 morphologies). PP intervals are irregular; most P waves are conducted to the ventricles though with varying PR intervals leading to irregular RR intervals creating a general impression of AF
● This rhythm usually occurs in older patients with COPD or congestive heart failure and may eventually develop into atrial fibrillation
● Digoxin and theophylline administration can be causally related
● Management is primarily that of underlying disease. Beta blocker is helpful if tolerated but is usually avoided because of associated obstructive airway disease. Non-dihydropyridine calcium channel blockers (diltiazem, verapamil) and amiodarone may be helpful. There is some evidence that IV magnesium may control the rate or even revert it to sinus rhythm.