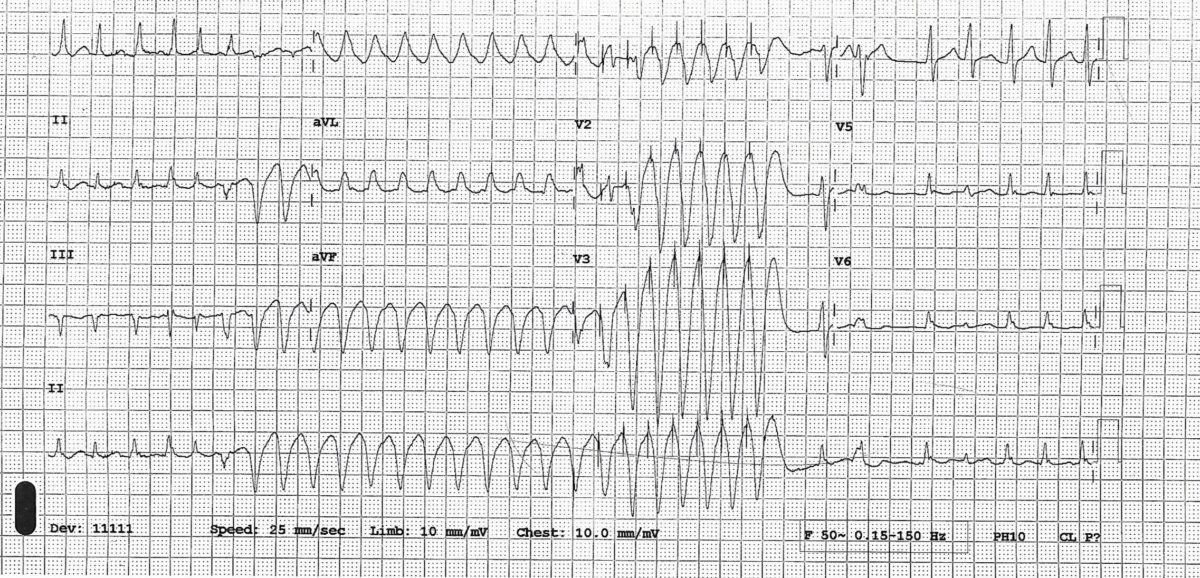
This is a straightforward but exceedingly rare ECG.
A 70-yr-old man presented with an episode of collapse. He was known to have severe LV systolic dysfunction and atrial fibrillation for a while. His coronaries were unobstructed, and his ECG showed-

As you can see ECG shows LBBB with right axis and atrial fibrillation. LBBB and right axis is a rare combination. LBBB is usually associated with normal or left axis. LBBB with right axis usually indicates biventricular enlargement and diffuse conduction system disease.
From a database of 636,000 electrocardiograms a series of only 36 patients with this combination was described. Most subjects had dilated cardiomyopathy with biventricular enlargement. (1)
References
1. Childers R1, Lupovich S, Sochanski M, Konarzewska H. Left bundle branch block and right axis deviation: a report of 36 cases. J Electrocardiol. 2000;33 Suppl:93-102.